Changes in UHC CLIA Policy
TNAAP has learned that UHC implemented a new edit on or around August 19, 2018 for physician (CMS 1500) claims when billing any type of lab services. Some providers may not have received this information. If you are having trouble with UHC claim denials for lab services, please see the policy changes below.
As always, TNAAP is here to help! If you are having any issues with claims, billing, coding, policies, etc., PLEASE Let Us Know!
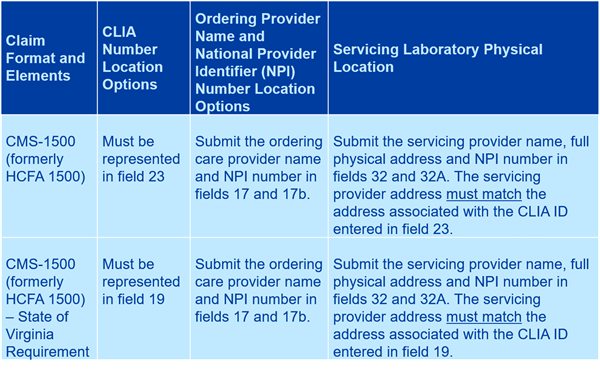
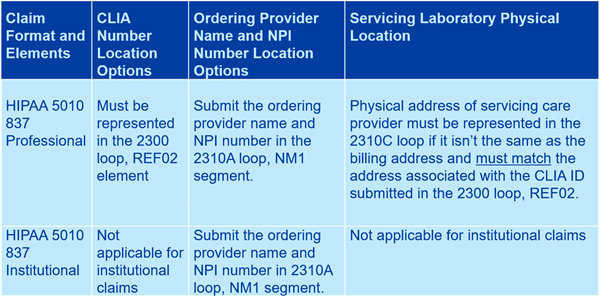
The new changes apply to any servicing care provider performing testing on biological specimens for the purpose of diagnosis or treatment is required to submit a CLIA ID. The servicing care provider is the care provider where the billed laboratory service was actually performed. In addition, the CLIA ID submitted must match the servicing location. The CLIA ID must be represented in field 23.
Clinical Laboratory Improvement Amendments (CLIA) ID Requirement Policy Update, Spring 2018, United Health Care
UnitedHealthcare’s CLIA policy:
Applies to:
All laboratory services subject to the CLIA submitted on either a CMS 1500 claim form or HIPAA 5010 837P claim file
Requires that:
All claims for laboratory services subject to the CLIA include the CLIA ID number for the servicing care provider and the servicing care provider’s physical laboratory address if that address is different than the billing care provider’s address listed on the claim
The billing or servicing care provider address submitted on the claim must match the address associated with the CLIA ID number.
Affects:
All lines of business
Contains:
Specific guidance around the claim’s submission process and CLIA-specific resource links.
We may reject or deny any claim as incomplete if it:
- Doesn’t contain the CLIA ID
- Is submitted with an invalid CLIA ID
- Is submitted without the complete servicing care providers demographic information
Claim line edits may also be applied if the provider’s CLIA certification type doesn’t support the billed service code.
Laboratory service providers who don’t meet the reporting requirements and/or don’t have the appropriate type of CLIA certificate for the services reported may not be reimbursed.
Applies to all laboratory services that are subject to the CLIA and submitted using:
- CMS 1500 claim form; or
- HIPAA 5010 837P claim file
Include the CLIA ID number for:
- The servicing care provider
- The servicing care provider’s physical laboratory address if it’s different than the billing care provider’s address listed on the claim
Check to make sure:
The billing or servicing care provider’s address you submit on the claim matches the address associated with the CLIA ID number.
Reference Materials
- UnitedHealthcare Commercial Policies: UHCprovider.com > Policies and Protocols > Commercial Policies > Reimbursement Policies for UnitedHealthcare Commercial Plans
- UnitedHealthcare Community Plan Policies: UHCprovider.com > Policies and Protocols > Community Plan Policies > Reimbursement Policies for Community Plans
Key Contacts
- Debra L. Locke, RN, MLT [ASCP], CPC, Process Consultant, UHC Payment Integrity/ Laboratory SME
- Shelly Woelfel, CLIA Program Manager, UHC Payment Integrity